5 Important Scientific Publications About Implant Dentistry

Table of Contents
Myths have been present since human civilization was described for the first time, and implant dentistry is sometimes subjected to some "myths".
It is nothing new. It´s human nature to create myths and incredible stories about what cannot be explained rationally.
In the medical field, some myths won't go away, like these examples:
- We only use 10% of our brains; hair and fingernails continue to grow after death.
- Shaving hair promotes new hair to grow back faster, darker, and stronger (I was sure this one was true 😂).
- Reading in dim light ruins your eyesight.
- People should drink at least eight glasses of water a day.
And the list goes on, and even physicians sometimes believe medical myths contradicted by scientific evidence.
We, dentists, also have our beliefs in some myths. The good news is that we read a lot of scientific literature, and only 5% don´t read it. Maybe I´m being too naive believing in this poll:
But yet, many dentists also believe that there is a lot of bias and commercial interest in scientific trials.
[Tweet "lot of dentists also believe that there is a lot of bias and commercial interests in the scientific trials."]
This article is not about dental myths in itself, but rather about a priori flawless and widely mentioned scientific publications that we should believe partially and conclude that there is no reason to trust blindly in everything that calls itself scientific research.
Let's start our list by describing why some publications should not be considered "word of God" and should be reviewed with a fine-tooth comb.
#1.The effect of inter-implant distance on the height of inter-implant bone crest.
Year Published: 2000
Primary Author: Dennis Tarnow
Cited by 859.
There is no doubt that the most adverse situation in implant dentistry is to have two adjacent implants if an aesthetic outcome is sought by the patient and clinician.patient and clinician seek an aesthetic outcome
I´m sure you have seen this situation very often in your dental office (unfortunately).
Below is a case I treated at my dental office, and as you can observe, there is no papilla between those two implants.
The main reason is that if you place the implants with an inter-implant distance less than 3 mm. the expected vertical resorption of the inter-implant bone peek crest will be more pronounced.
Tarnow, in 2003, proved that the expected height of the papilla between two implants is around 3.4 mm.
This limitation in the height of the papilla in the aesthetic zone can be a drama.
[Tweet "This limitation in the height of the papilla in the aesthetic zone can be a drama."]
What is an excellent article (Tarnow 2003), sort of methods used in this article should be discussed:
- It was performed using different implant systems. Therefore, it is not the same one-stage or non-submerged philosophy implant compared with a submerged or two stages implant philosophy.
- Also, different surfaces were included (turned, titanium dioxide blasted, titanium plasma sprayed, sandblasted, and acid-etched and sandblasted and the behavior of the other surfaces topography is different (Alomrani 20005).
- It measured the papilla in molars, premolars, and anterior teeth implants.
- The measurements were performed with a periodontal probe and were rounded off to the nearest millimeter, and standard deviations were not included in this investigation.
Although this study is one of the most mentioned studies in the history of implant dentistry, we should also read other studies where results may be more accurate, and the methodology used to obtain the data is more concise (Gastaldo 2004).
Also, we should consider that the results may vary if implants with Platform Switching are used (Ciurana 2009), and implants may be closer to each other by less than 3 mm, and achieve an improvement in the preservation of the interimplant bone crest.
The point is that the distance between the implants is not the most important: It is the distance between the implant connection that matters.
[Tweet "distance between the implants is not the most important: It is the distance between the implant connection"]
When there is a mismatch that increases the distance between the two conflictive zones (implant connections), the more closely these implants can be placed.
And if the interimplant bone crest is preserved...maybe there will be an improvement in the height of the papilla between two adjacent implants...or maybe not.
We should consider having a distance between the contact point of the restoration and bone peek crest inferior to 3 mm to achieve a total with papilla between restorations.
This animation explains the publication from Ciurana in 2009 and why it is essential to consider the distance between implant connections rather than the distance between implants.
Tip to avoid unpleasant complications using multiple implant restoration in the aesthetic zone: 1 implant and two restorations (1 pontic restoration with cantilever).
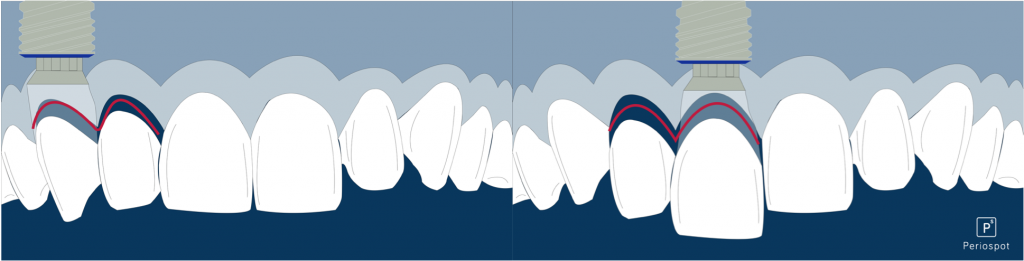
Fig. 1- Two different options to restore two missing teeth in the aesthetic zone, avoiding two adjacent implants.
#2. Resorption of the buccal and lingual bone walls of fresh extraction sites following implant installation
Year Published: 2006
Main Author: Araújo & Lindhe
Cited by 337.
A lot to say about this article. And not flattering things.
I think this article was created to "demonize" immediate implants.
I cannot understand how this article is so important for many researchers and serves as a reference to discard or underestimate authors that did good research about immediate implants and validated it as an option for our daily practice.
First, they used wide implants in sockets where these implants could barely be placed without engaging the buccal wall.
That´s why in the histologies it is observed remarkable resorption of the buccal bone wall.
Also, they raised a flap to place these implants. Other researchers proved that raising a flap in immediate implants promotes soft tissue recession (Blanco 2008).
In the animation below it is shown the difference between the Araújo and Blanco research:
This research was performed on dogs. We will talk later in this article about other studies about immediate implants performed in humans.
#3. Patient selection and preparation. Tissue-integrated prostheses
Author: Lekholm & Zarb
Year: 1985
Citations: 2359
In this article, Lekholm and Zarb propose a bone classification where four types of bones were identified:
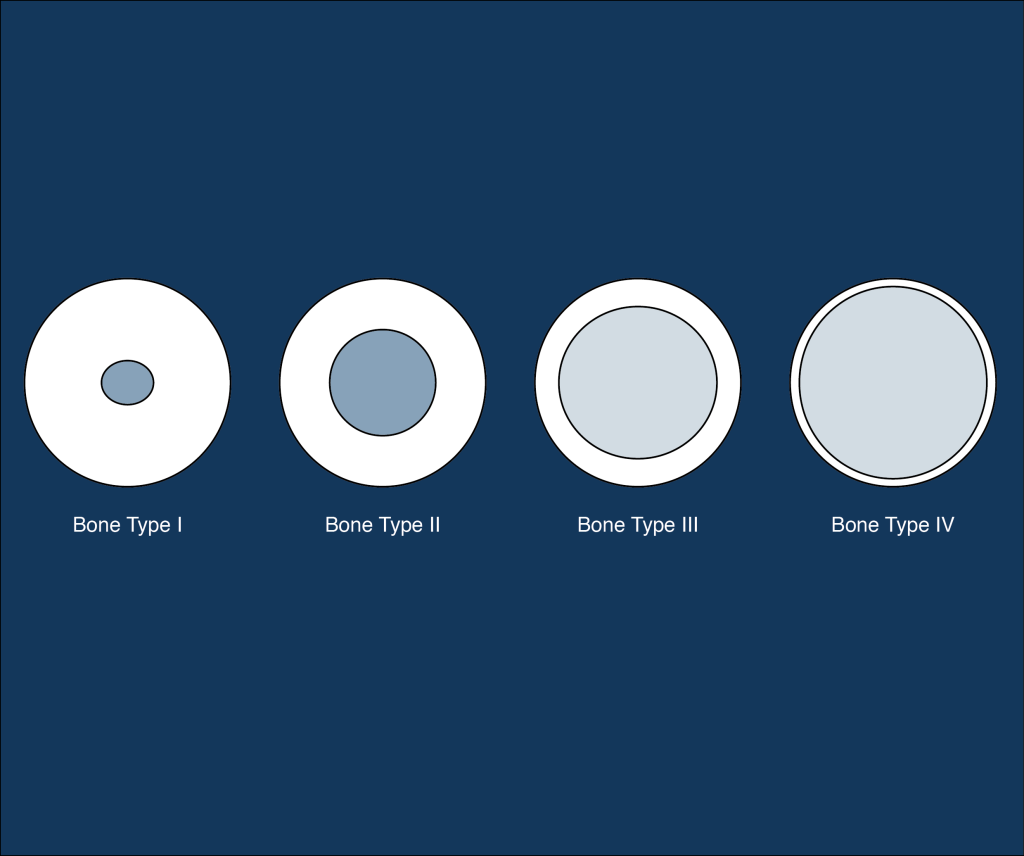
The bone quality classification was proposed by Lekholm & Zarb in 1985.
- Type 1 bone in which almost the entire bone is composed of homogenous compact bone.
- Type 2 bone is a thick layer of compact bone surrounding a dense trabecular bone core.
- Type 3 bone in which a thin layer of cortical bone surrounds a core of dense trabecular bone.
- Type 4 bone is characterized as a thin layer of cortical bone surrounding a core of low-density trabecular
bone of poor strength.
This classification is widely accepted and used in several Congresses, courses, and other training sessions to address bone quality.
Bad news came when some authors tried to find a relation between that bone quality classification and histological analysis (Trisi & Rao 1999).
It is tough to identify the difference between type II and type III bone from a histological and preceptory point of view (Trisi & Rao 1999).
[Tweet "It is tough to identify the difference between type II and type III bone"]
So we could say that there are only three types of bone:
- Soft bone.
- Medium bone.
- Hard bone.
But no one gives a damn about this fantastic article, and nobody mentions it in congresses and courses.
Speakers and authors rather stick to the standard and more widely accepted Lekholm & Zarb classification (except Daniel Rodrigo and I learned it from him).
Next time you listen to someone mention the Lekholm & Zarb classification, please let him know there are other options to assess bone quality.
Also, you can read more about this in this post about immediate loading.
#4. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans.
Author: Iasella
Year: 2003
Citations: 583
No doubt that alveolar ridge preservation is a predictable treatment option when treatment with implants is going to be performed after an extraction.
This approach counteracts the events that take place after an extraction that is well described in several articles (Cardaropoli 2003, Araújo & Lindhe 2005), without preventing the physiological resorption that always happens when the blood supply from the periodontal ligament to the bundle bond is eliminated (Ten Heggeler et al. 2010).
Events that take place after extraction are well explained in this animation (Cardaropoli 2003):
Iasella, in his article, performs ridge preservation with some peculiarities:
- Raises a flap without achieving wound primary closure.
- Include non-molar teeth. Premolars were included where the buccal wall is expected to be thicker than canines and incisors (Januario 2011).
- Uses a membrane.
- The biomaterial to fill the socket was allograft.
The result was that ridge preservation improved the results obtained when no ridge preservation was performed.
But the most peculiar aspect of this article is that there is a vertical gain of 1.3 mm on the preservation group, which in the aesthetic zone means a lot.
Regarding these results, we could say that the Iasella procedure is the "gold standard" for alveolar ridge preservation, but there is some data that we should also consider: Standard deviation.
That vertical augmentation of 1.3 mm has to be taken with caution cause the standard deviation was +/- 2 mm.
Also, these results could be due to the overfilling of the socket with the bone substitute (37% was no vital bone after histologies were taken).
When performing alveolar ridge preservation, we should consider other procedures like the one reported by (Jung 2004, 2012), without raising a flap and using a xenograft with 10% collagen (Bio-Oss® Collagen) covered whether with an autograft from the palatal or a collagen matrix (Mucograft®).
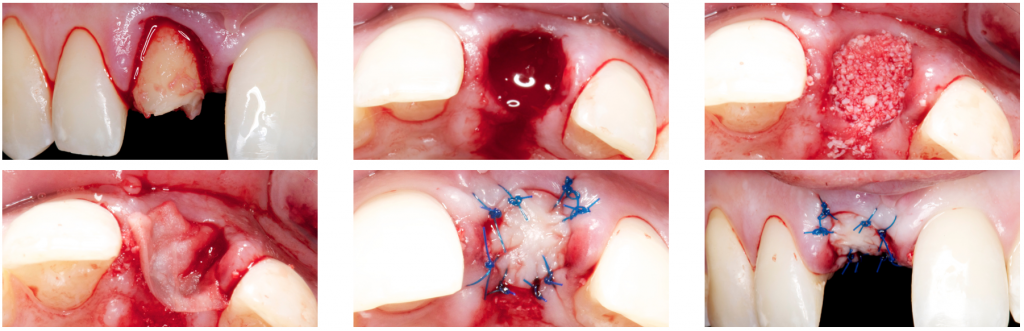
Ridge preservation using Bio-Oss®, Bio-gide®, and a soft tissue graft from the palatal to cover the socket.
These procedures published by Jung have been proven to be a reliable and predictable option when a treatment involving implants will be carried out after an extraction.
#5. Immediate versus delayed implant placement after anterior single tooth extraction: the timing randomized controlled clinical trial
Author: Tonetti
Year: 2017
Citations: 0
Quoting partially, the conclusion is already scary "Immediate implant placement should not be recommended when aesthetics are important."
This is a quite daring conclusion.
Immediate implants in dentistry have been discussed in the last 15 years in almost all congresses and important events about implant dentistry.
It is a controversial topic.
But there are some points we should highlight about this RCT:
- A flap is raised to place the immediate implants, which we already know from the literature that this has a negative impact compared with the flapless approach (Blanco 2008, Fickl 2008).
- No provisionals were used after immediate implantation. The use of provisionals may have a positive role in maintaining the soft tissue architecture when replacing extracted teeth (Kan 2001, Kan 2003, Kan 2005, Rouck 2008, Cabello 2013).
- The distance between the implant and the buccal bone wall may not be adequate.
- Data from the studies show that maybe only a small gap was left between the implant and the buccal wall—a lot of heterogeneity among the socket morphology in the immediate implants group.
- There are more regenerations in the immediate implant group than in the delayed group (72% vs. 43.9%). GBR at the time of immediate implant is a very sensitive technique.
Although this RCT is a strong and solid trial, we should read it carefully cause the conclusion of this article may lead us to think that immediate implants are totally unpredictable.
The key is when to choose to place immediate implants and the experience of the clinician performing the case. You can find some basic rules here in this article about immediate implants.
[Tweet "The key is when to choose to place immediate implants and also the experience of the clinician"]
Conclusions:
Scientific literature is necessary to help us clinicians to establish evidence-based clinical practice.
We can find some bias when we carefully read articles that are the most cited in the scientific literature or congresses about the topic implant dentistry and periodontics.
That´s why it is important to read the discussions of more recent articles where older articles are analyzed and mentioned.
The article cited above is a reference to our daily practice, but we also should sometimes question ourselves if these scientific publications should be blindly followed.
What other well-known articles about periodontics and implant dentistry should this list include?
Recommended Book (also visit the Periospot reccomended books about implant dentistry)
Comments
0 totalLoading comments...
Previous
3 Suturing Techniques For Guided Bone Regeneration That You Can Start Using Tomorrow
Next
Socket Shield Technique. Report of a case.
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
13 min read
