The Ideal Implant Position in the Aesthetic Zone.

Table of Contents
Jim Collins, the author of the book Good to Great, once said,
"The main point is to first get the right people on the bus, and the wrong people off the bus, before you figure out where to drive it."
He was implying that good-to-great leaders understand three simple truths. First, you must begin with "who" rather than "what".
In this book (by the way, my favorite book about business), Jim Collins presented research where he analyzed why some companies remain "Good" and how some companies can take the leap from "Good to Great."
If you invested $1 in a mutual fund of the good-to-great companies in 1965, holding each company at the general market rate until the date of transition, and simultaneously invested $1 in a general market stock fund, your $1 in the good-to-great fund,withdrawnon January 1, 2000, would have multiplied 471 times, compared to a 56-foldincrease in the market.
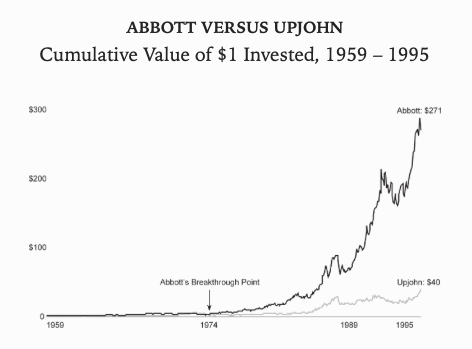
Not bad! Now I wish I had invested 1000€ in Abbot.
Before we start, we must apply the principles, mentioned above, to Implant Dentistry, considering:
- What materials we are going to use.
- What we know about implant biology.
- Surgical techniques and skills.
Firstly, we have to understand the implant system that is currently in use. Is it an internal connection? What is the expected marginal bone loss? What is the resistance to the fatigue of the implant?
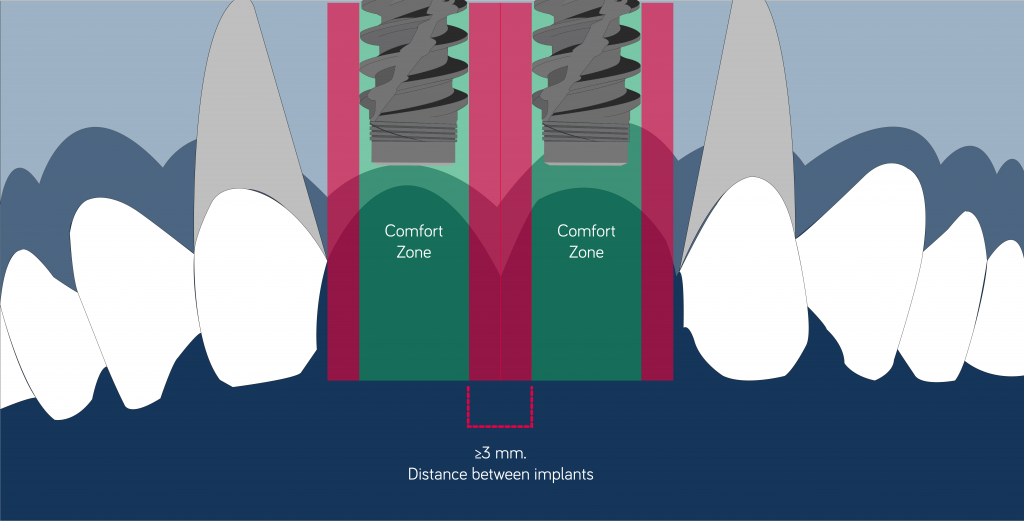
What do we know about implant biology? What is the minimum distance between the teeth and the implant? Or between two implants? Why is there a "safe zone" to place an implant? What biological implications does this "safe zone" entail?
Am I prepared to solve critical situations when it comes to ideally positioning an implant?
Should the implant be placed where the bone is available, or where it makes sense from a prosthetic point of view?
Am I prepared to solve situations where there is a lack of soft tissue/bone available to guarantee a proper implant position?
Before beginning, we must make sure that we use the right materials (the right people).
Additionally, we must make sure that we have comprehensive knowledge about implant biology (the right people in the right place of the bus).
Finally, we must be sure to know how to use this knowledge and material to our patient’s benefit (we must know how to drive the bus).
The goal of placing the implants in an ideal 3D position is to:
- Avoid damaging the bundle bone,and minimize its resorption.
- Maintain the correct distance between adjacent teeth/implants in order to preserve adequate blood supply, and maintain healthy hard and soft tissue.
- Allow a correct prosthetic phase.
Mesiodistal position.
It is mandatory to keep a distance of 1.5 mm between the implant and the adjacent teeth (Tarnow 2000).
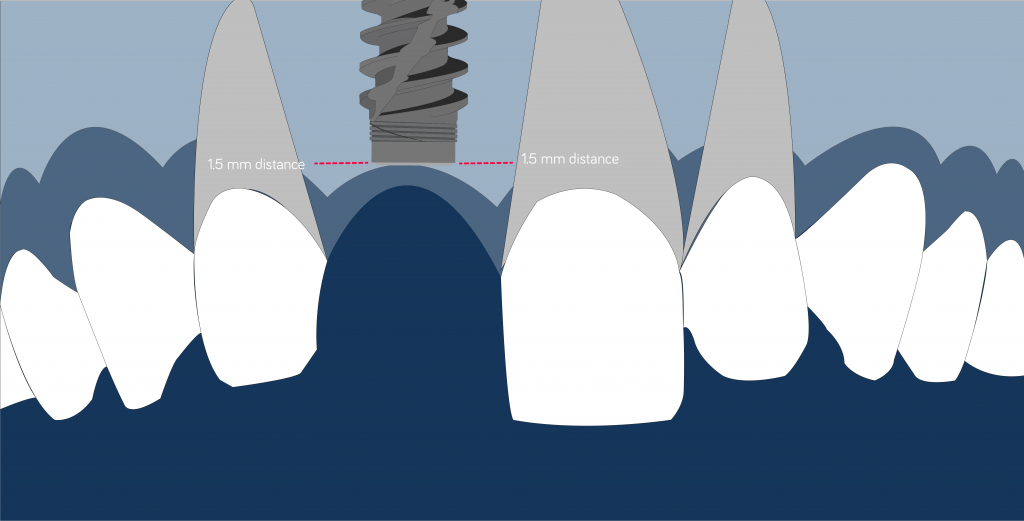
This distance will protect the interproximal bone peak from being affected by the "saucerization effect" that takes place when the biological width is formed.
The inflammatory reaction that takes place around the gap, between the implant and the abutment, produces an inflammatory response that is likely to create marginal bone loss to an average extent of 1.5 mm (Berglundh 1991, Ericsson 1995).
If this marginal bone loss affects the proximal bone peak, it will be resorbed and the presence of the papilla, between the future restoration and the teeth, will be improbable.
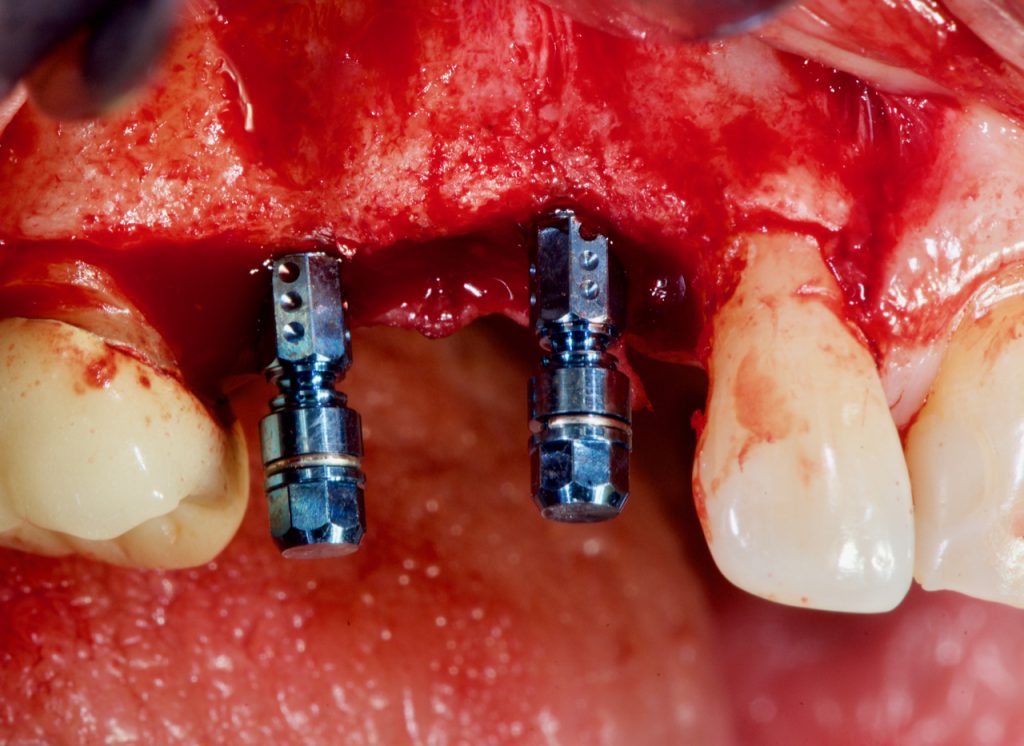
This rule also applies to implants where a distance of 3 mm should be kept so as to avoid the merging of the “saucerization effect” of the two implants which would lead to a collapse of the interproximal papilla (Tarnow 2001).
Some recent publications stated that this rule might not be valid when Platform Switching implants are used.
There is an entire article, here, on Periospot, dedicated to Platform Switching (Ciurana 2009).
We must bear in mind that the absence of the papilla is not only an aesthetic problem; however, it also implies phonetical consequences,
Other, less biased, research proved that increasing the distance between two implants or between the implants and teeth (3-4 mm) would increase the probability of the presence of papilla.
Some tools exist that can help to avoid placing implants at too close a proximity.
This tool is very popular and is widely used to support the placement of the implants in a proper mesiodistal situation.

Buccolingual Implant Position
The first rule, regarding the buccolingual position, is about the amount of bone that should surround the implant.
The thickness of bone on the buccal side should not be less than 2 mm (1.8 mm).
This is the minimum thickness that the bone needs to be in order to avoid being resorbed when it doesn't have a supply of blood from the periodontal ligament (Spray 2000).
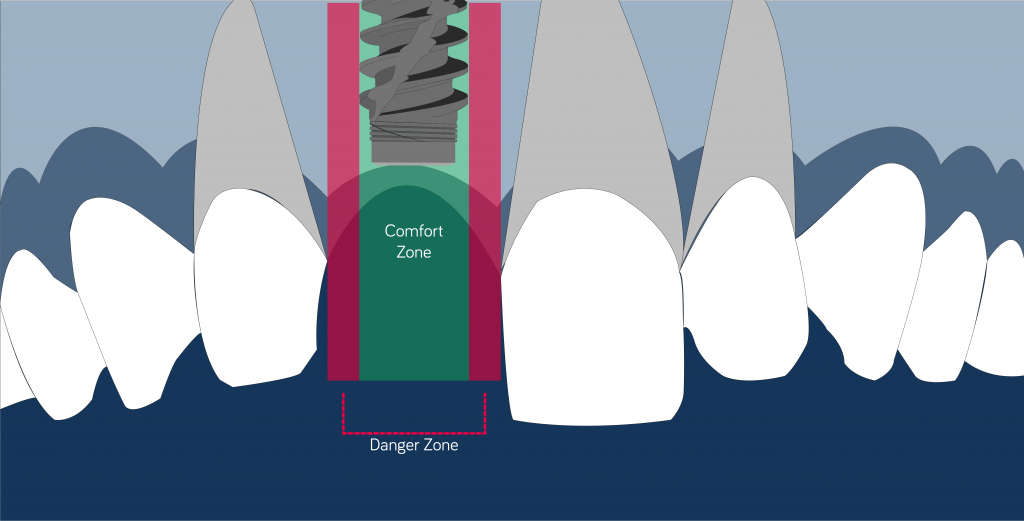
In the aesthetic zone, the implant should emerge at 1.5-2 mm from the ideal point of the emergence profile. This "comfort zone" was described by Buser in 2004.
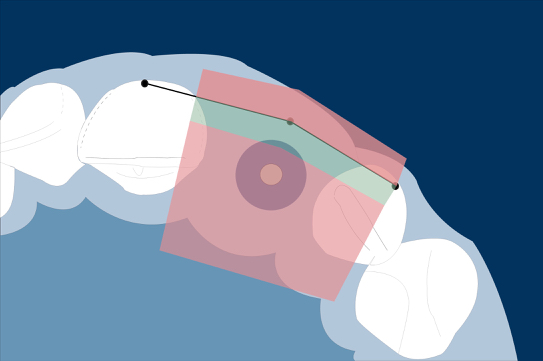
We can draw an imaginary line connecting the buccal points of the emergence profile to ensure a proper implant position.
An implant that is placed too buccally may have aesthetic complications like soft tissue recession, larger restoration, soft-tissue discoloration, and other biological complications that can lead to peri-implantitis.

Video removing the implant above.
Regarding the ideal 3D position, when an immediate implantation is performed, it is essential to evaluate the sagittal situation of the root.
To help us in this evaluation, we can use the classification published by Kan. This video summarizes the four classes (Kan 2011):
In this article, you can find more content about immediate implants in the aesthetic zone.
In a narrow ridge, TiZr implants are a very good option to avoid extra procedures with guided bone regeneration.
Using Roxolid® implants (Straumann, Switzerland) is an alternative option to avoid enlarging the treatment time and reduce the invasiveness of implant treatment.

Below the video of the surgery involving Roxolid® implants.
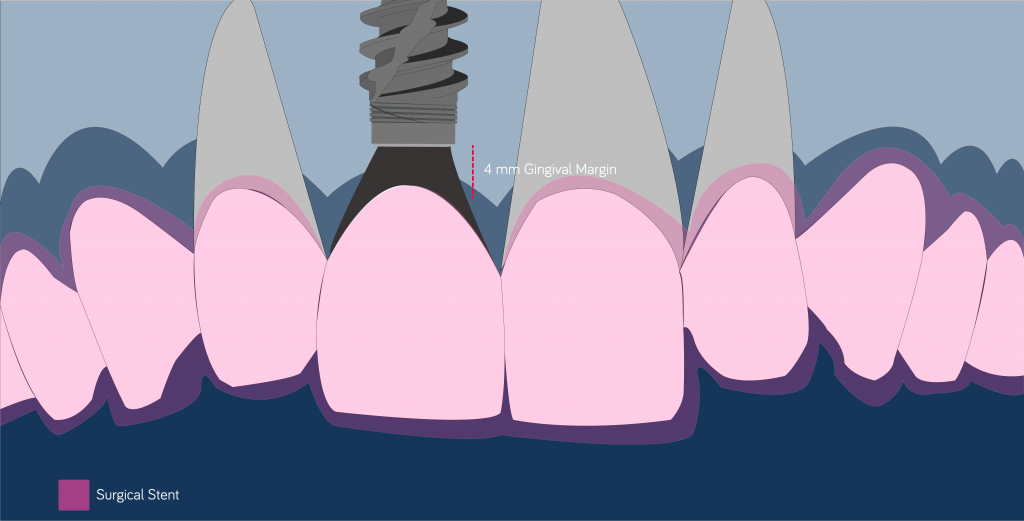
The Corono-Apical Position
Placing the implants below the bone crest may have advantages from a biological and prosthetic standpoint.
But once again, before placing an implant in a subcrestal position, we must know the kind of connection we are managing.
Cone Morse Connections have been proved as a suitable option to be placed in a subcrestal position.
Placing the gap below the bone crest can lead to a peri-implant reaction along with marginal bone loss, therefore affecting the final soft tissue contour.
As a general rule, the implant should be placed 3-4 mm below the gingival margin of the future restoration.
By using a surgical stent that is based on a wax-up, reproducing the desired final restoration is mandatory to achieve optimal Corono-Apical positioning.
Conclusion
A Summary of some of the points described:
Mesiodistal position: The implant should be placed 1.5 mm away from the adjacent teeth. If possible, it should be placed 2 mm away to stop the marginal bone loss from affecting the interproximal bone peak.
The distance between implants should be 3 mm, although some authors stated that Platform Switching implants could be placed up to a distance of 2 mm (Ciurana 2009).
Buccolingual position: The general rule claims that at least 2 mm of bone should be present around the implant — more attention should be given to the buccal side where buccal bone resorption will lead to aesthetic failure.
The alveolar bone, which doesn't receive a supply of blood from the periodontal ligament, needs a width of at least 1.8 mm to not get resorbed.
Apico-Coronalposition: The implant should be placed 3-4 mm below the gingival margin of the future restoration. Implants that are placed too coronally will not have enough room for the emergence profile.
Now that we have a clear picture of how implants should be placed in the aesthetic zone, we can choose the right materials and place them in a proper position.
The dentist is responsible for driving the bus with the right people (implants), and seating them in the right position (biological knowledge).
When several implants have to be placed in the aesthetic zone, other factors should be considered.
In this article about different options to restore the aesthetic region with multiple missing teeth, there is more information about the biological and biomechanical rationale behind each option.
In the Corono-Apical position, a surgical stent should be used to provide a vision of the future restoration related to the implant position.
Also, for the Mesiodistal position, tools like this can help to avoid placing an implant too close to a tooth or another implant.
Hope you found this article useful and if you have any remark you would like to share, please leave a comment below.
Recommended Book- Implant Therapy in the Esthetic Zone.
Comments
0 totalLoading comments...
Previous
How to create Animations and Illustrations to Improve your Presentations.
Next
6 Tools to Boost Your Online Dental Marketing
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
13 min read
