4 Techniques to Perform an Effective Ridge Preservation and Soft Tissue Management

Table of Contents
I started to get interested, in detail, about Alveolar Ridge Preservation and Soft Tissue Management about 7 years ago when I was asked to write a chapter in the 3rd edition of “Periodontal and peri-implant plastic surgery” by Dr. Alain Borghetti and Pr Virginie Monnet-Corti.
And that's the topic I chose to start my collaboration with Periospot. I'm excited to join this team, representing France, and I'm sure you will have more articles about the implant and plastic periodontal surgery.
This work allowed me to become aware of the importance of biology in our implant treatments: as is known, it is widely described in the literature: once a tooth is extracted, the bone resolves inexorably... but what we know today is that even implementing a technique for preserving bone volume... this resorption persists and can lead to very critical aesthetic situations if it is not anticipated!
Filling an alveolus is not a very technical, but managing the soft tissue that must protect this filling is much more so.
The interest of this article is twofold:
1- Understand and learn 4 post-extraction soft tissue management techniques.
2- Implement a technique that can compensate for the buccal bone loss, such as the saddle connective tissue graft, my favorite technique in the anterior region!
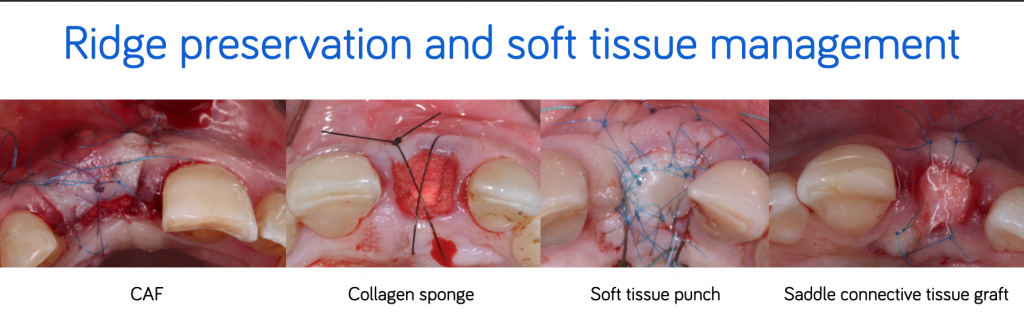
Ridge preservation and soft tissue management
The placement of a bone-filling material significantly reduces vertical and horizontal post-extraction resorption (Araújo et al., 2015) (Sanz et al., 2015) (Mardas et al., 2015).
Barone et al. (2012) and Festa et al. (2013) show a decrease in resorption of 1.97 mm in width and 2.6 mm in height for sites filled by a biomaterial compared to unfilled sites.
However, bone resorption is predominantly in the vestibular coronary third (Chappuis et al., 2013). Januario et al. (2011) show that the bony bone table in the anterior maxillary area is thin (0.6 mm on average and less than 0.5 mm in more than one case out of two) and that the more the cortical bone is thin, the more its resorption is important.
To protect the blood clot and the filling material and to optimize the preservation of the tissue volume, several surgical techniques make it possible to close the socket:
- The coronally advanced flap (CAF)
- The collagen sponge
- The soft tissue punch
- The saddle connective tissue graft.
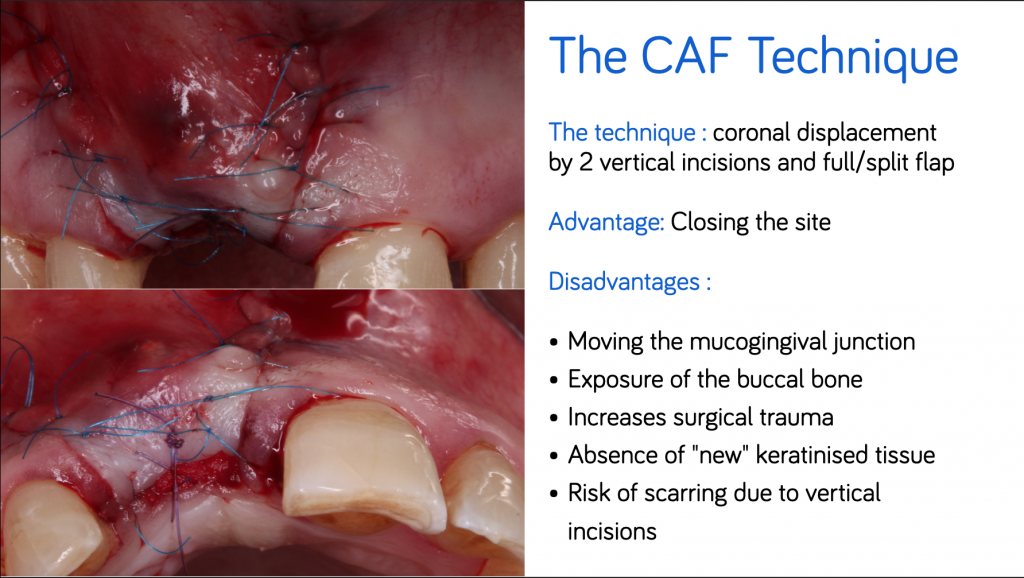
#1. The CAF
The CAF provides healing by first intention. It involves the realization of two incisions of vertical discharges and an incision in a partial thickness of the buccal flap, which strongly reduces the vascular supply.
From an esthetic point of view, incisions of discharges can cause visible scars in a patient with a line of the high smile as well as a displacement of the mucogingival line.
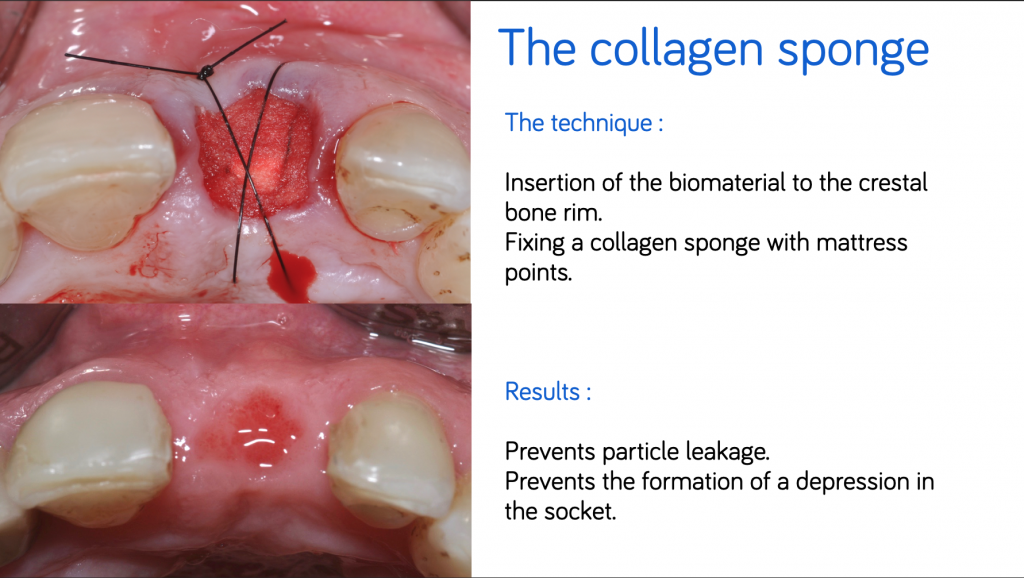
#2. The collagen sponge
Collagen sponge or "Bio-Col" technique (Sclar, 1999) consists of the insertion of a bone filling material to the crestal rim and the closure of the socket by a collagen sponge fixed by padding points.
Collagen prevents the infiltration of connective cells into the coronal portion of the socket and guides healing to prevent the formation of depression into the socket.
#3. The soft tissue punch technique
The soft tissue punch (Landsberg and Bichacho, 1994) (Jung et al., 2004) is removed from the palate or from the maxillary tuberosity.
The tuberosity sampling makes it possible to obtain a greater graft thickness and a lower post-operative sensitivity. However the tissue is more fibrous is less vascularized which can hinder its healing.
A palatal sample is therefore recommended: it is performed with the knife blade (No15, 15 C) or with a circular knife provided for this purpose.
The protection of the sampling site is identical to an epithelial-connective sampling technique with a hemostatic material and fixation sutures.
The punch is positioned directly in contact with the biomaterial, so its vascular supply is very low and the morbidity of this therapy is high (Thalmair et al., 2010).
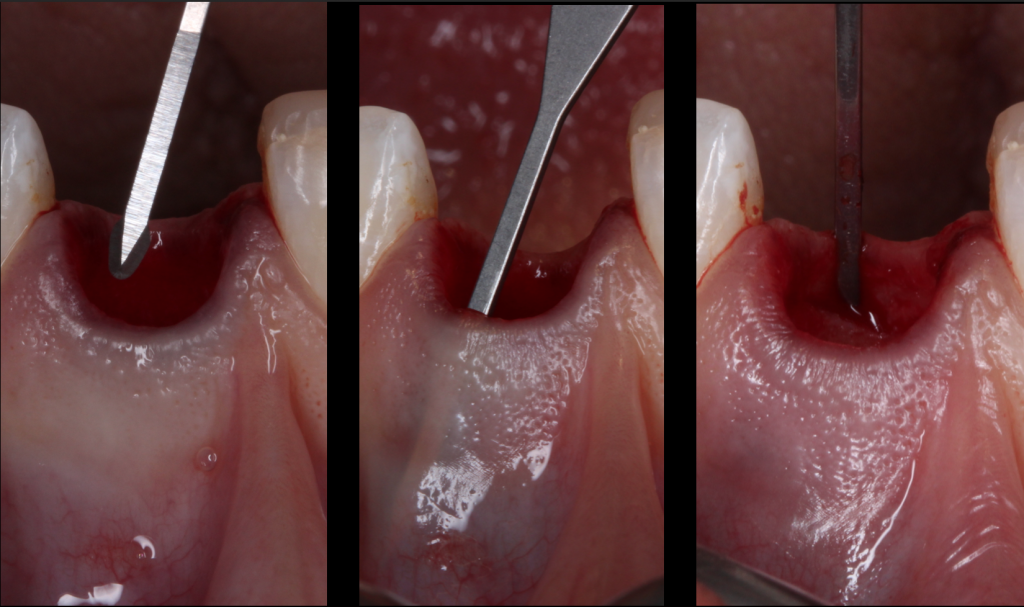
The principles of this technique are :
- Atraumatic extraction with preservation of the marginal periodontium
- Suppression of the sulcular epithelium with the diamond bur or the scalpel blade to increase the vascular supply
- Removal of almost the entire thickness of the palate
- Punch size slightly higher than the recipient site
- Adaptation and immobilization of the punch with several simple points
- Tissue maturation is about 3 months (Thalmair et al., 2013).
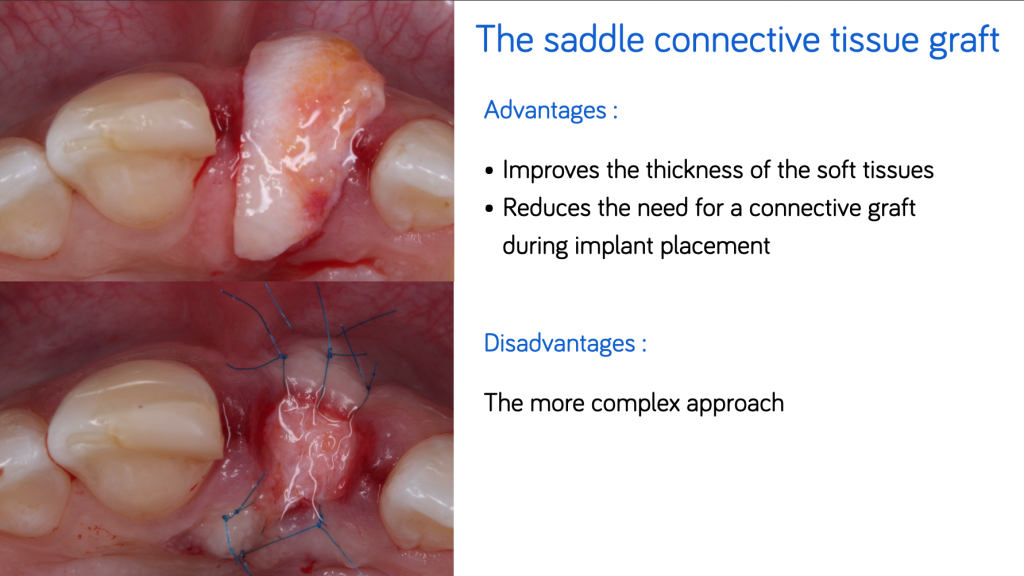
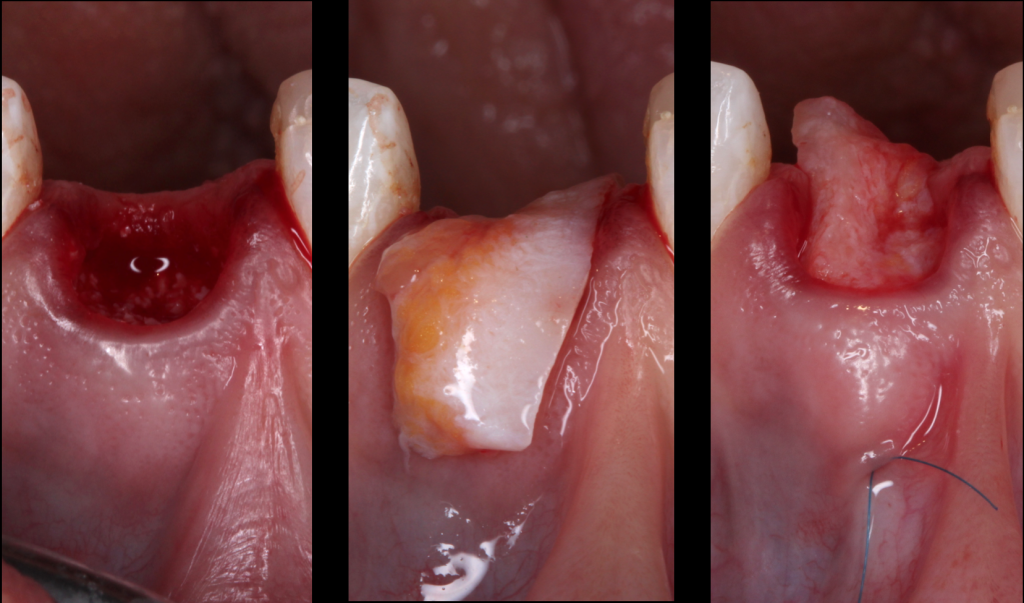
#4. The saddle connective tissue graft
The saddle connective tissue graft associates closure of the extraction site with an increased volume of soft tissues in the buccal part (Chen and Dahlin, 1996).
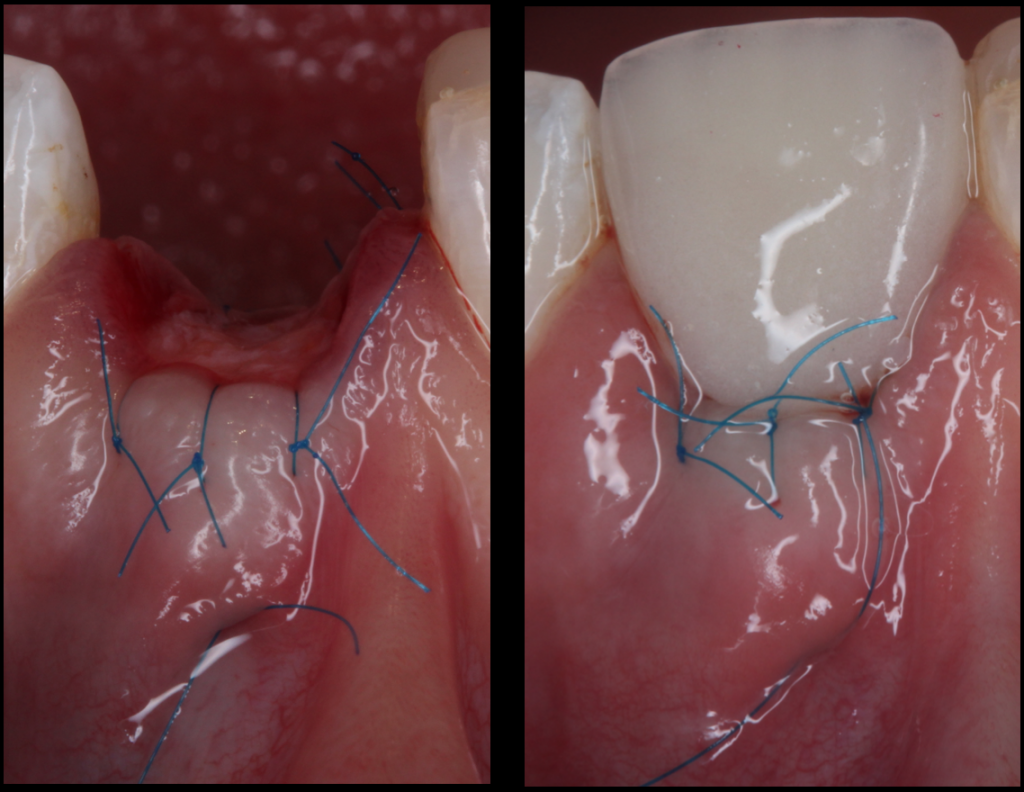
The graft is positioned in the vestibular and palatal which involves the realization of a buccal supra-periosteal envelope (about 5mm) and a palatal detachment (about 3mm) to introduce the connective graft while preserving the papilla (Fig.5).
The increase in the thickness of the buccal gingiva makes it possible to compensate for the irreversible loss of bone volume despite the filling, and thus to obtain the best horizontal and vertical preservation of the soft tissues (Vanhoutte et al., 2014).
This approach, which is more complex, increases the quantity of soft tissues, particularly in the case of a fine periodontal phenotype, and thus reduces the need for a connective graft during implant placement. Some authors recommend keeping an epithelial area on the exposed part of the graft.
Clinical Case





Surgery Video
Conclusion :
When implemented, filling techniques significantly reduce the need for complementary surgical techniques (Mardas et al., 2015).
The healing time required for bone filling before implant placement is variable depending on the study and ranges from 4 to 9 months.
This time must depend in particular on the importance of the bone filling done and the cofactors that can influence the healing (tobacco, diabetes ...).
In the majority of the studies, a healing time of 4 months is respected before the installation of the implant: the filling causes a delay of healing in the first phases of the post-extraction bone regeneration. Even if the regeneration is not complete, the placement of the implant will not interrupt it.
The respect of the time of osseointegration makes it possible to obtain a final healing time of 7 to 8 months before the realization of the prosthetic phase.
The essentials of pre-implant alveolar filling :
- Put an osteoconductive bone material with a low degree of resorption.
- Isolate the biomaterial of the conjunctival epithelial cells to avoid encapsulation.
- Close the extraction socket and stabilized the clot.
- Disrupt as little as possible the vascular supply by an atraumatic intervention.
Recommended Book
Plastic-Esthetic and Implant Surgery

Comments
0 totalLoading comments...
Previous
Zero bone loss concepts by prof. Tomas Linkevičius. A path to crestal bone stability
Next
Low Budget Overhead Video Guide: Recording Dental Procedures Effectively
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
13 min read
