Introduction
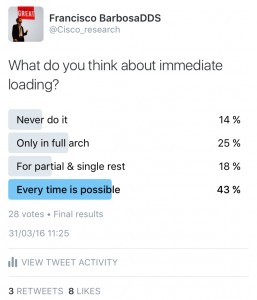
Once again, before I start writing this post, I did a poll on Twitter about immediate loading:
And it seems that dentists they do love immediate loading…or perhaps, their patients love it even more.
When we talk about immediate loading, maybe a lot of definitions may come to our mind.
Does it means that the restoration is delivered the same day of the surgery?
Does it means that the restoration has occlusal contact?
To answer these questions, we have to talk about the latest Consensus about this topic.
To achieve a consensus amongst dentists is harder than run backward wearing sandals. If you don´t believe me, just join a discussion in a Facebook group.
And immediate loading is a concept that is subject to this controversy.
Let´s take a look at the evolution of this concept:
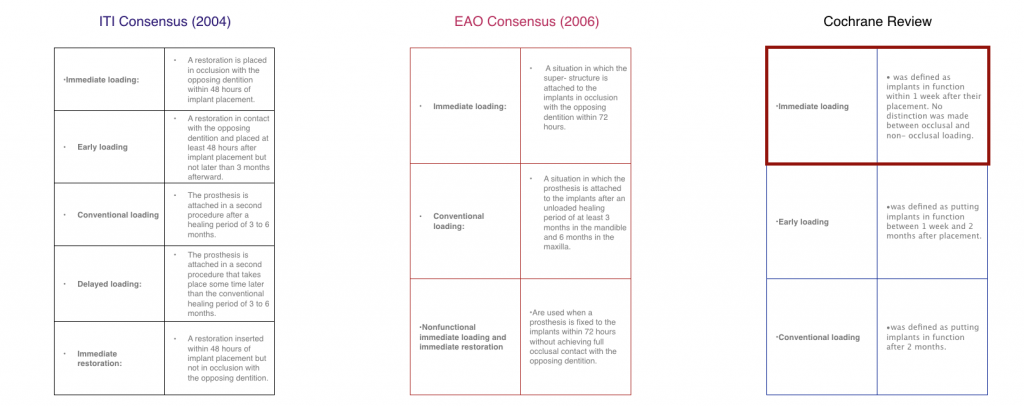
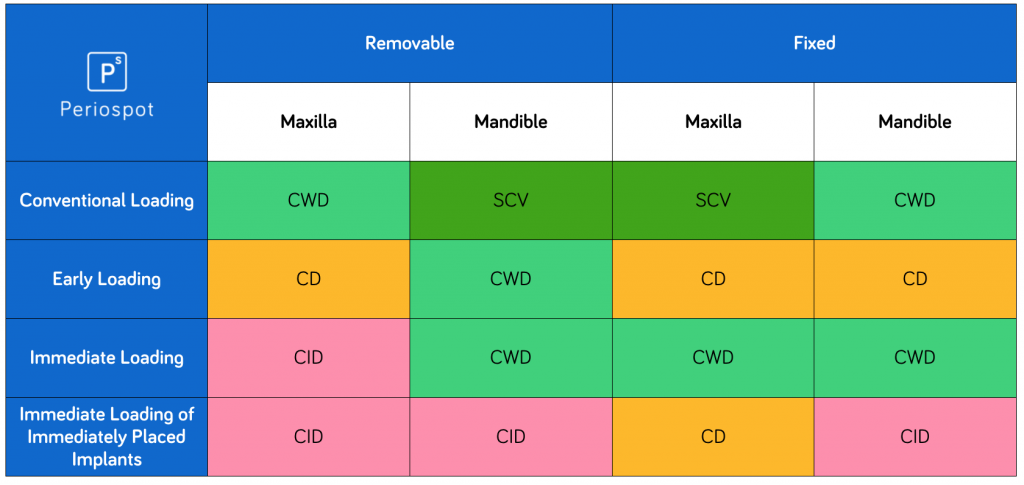
The box with the latest accepted definition is marked above. In the last ITI consensus, this was also the accepted definition (Gallucci 2014).
If we consider immediate loading as being earlier than 1 week subsequent to implant placement, with or without occlusal loading, is it correct to say that one stage surgeries could be considered immediate loading?
Some authors defined the pseudoloading, something that we should consider and avoid, in those implants with low primary stability (Touati 2002).
Our patients, they do love to chew with the healing abutments. Remember that.
Biological considerations regarding immediate loading
I´m going to be short here, because I want to create another post only about this topic.
While the original Brånemark protocol advocated the use of a two-stage surgical approach, in Switzerland, Dr. Schroeder started with the development of titanium plasma-sprayed implants for one stage approach, with a predictable result (Buser 1990).
Ledermann was the first performing immediate loading, using 3-4 implants in the anterior mandible (Ledermann 1979).
Nevertheless to say that these implants had a mandibular bicortical anchorage.
But what are the factors that lead an implant to osseointegration, or to fibrointegration?
The rationale behind immediate loading is reducing the risk of fibrous integration. At the same time, it is important to promote the formation of the lamellar bone, that sustains a continuous occlusal loading.
To make a quick reminder, lamellar bone is organized, highly mineralized, and is the strongest bone type.
Woven bone is unorganized, less mature, less mineralized and has lower strength and is more flexible.
After placing the implant, the lamellar bone that surrounds the implant is substituted by woven bone.
Woven bone formation by appositional growth may start to form as early as the second week after implant placement (Berglundh 2003).
We can see the sequence in this video:
We have to keep in mind that during the week I and week IV, the bone immediately in contact with the implant, is resorbed in some areas.
Approximately 3-5 weeks after implant placement, the implant-bone interface is weakest and at highest risk of overload since the implant-bone interface is least mineralized and unorganized during this time (Turkyilmaz 2015).
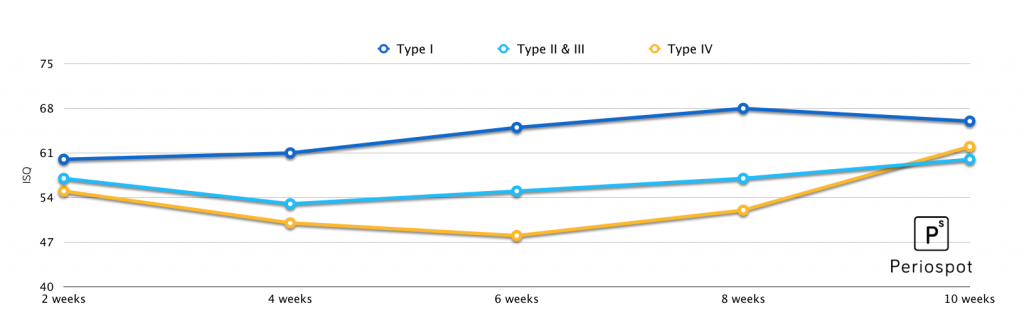
This means that the initial mechanical anchorage is gradually substituted by biological stability (Barewal 2003).
This chart explains the idea:
The importance of performing a RFA assessment to implants, is that we have a value (ISQ), thats is directly related to the implant resistance against micromotion (Brizuela-Velasco 2015).
The accepted range of micromotion, accepted during the healing phase, is between 50-150 µm. When this threshold is trespassed, the implant will be encapsulated by a fibrous layer (Szmukler-Moncler 1998).
Summarizing: It is not the time of loading that may lead to implant failure. It is the presence of micromotion (>50-150µm) at the implant interface, during the healing phase, that may cause implant failure.
Depending on the treatment approach, different scientific support can be found.
Now let´s move to the clinical batch.
Considerations in the initial examination in immediate loading
I already wrote about some of these considerations here in this post, about immediate implants.
To summarise, these are the keypoints before start planning a case:
General aspects:
– Patient motivations and perspective
– General health status
– Etiology of the patient´s edentulism.
– Age
– Extraoral examination (smile line and facial support)
Intraoral examination
– Hygiene
– Periodontitis: here I have to stop. Periodontitis must be treated before any implant is placed in the patient. There is a strong correlation between periodontal disease, and peri-implantitis (Karoussis 2004, Lindhe 2008).
You can check here more about peri-implantitis and its epidemiology.
– Acute infection
– Jaw opening
– Interarch relationships
-Morphology of the edentulous bone crest
– Quality and quantity of the soft tissues
Treatment Plan
This point can fill by itself a book chapter, so I´m going to focus only on two points (we will see more about this specific step in other posts):
Facial and lip support
When a patient wears a removable denture, usually this kind of prosthesis provide sufficient lip support.
We have to maintain the lip support with the new prosthesis.
2 ways to address this issue:
– Maintain or improve the actual design. In case of an overdenture, the lip support is easily enhanced.
– Provide lip support with an alveolar bone augmentation (Lorenzo 2012). The idea is to provide support through the use of biomaterials placed buccally.
You can see the technique in this video.
This technique is very useful, and when the patient is strongly motivated in favor of a fixed rehabilitation without a buccal flange.
Also, there is a full chapter about this on this iBooks.
A short video about this first tip:
Bone quality assessment before surgery
I have some bad news here:
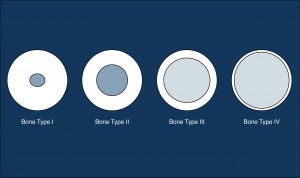
“Lekholm & Zarb classification is not useful (Lekholm & Zarb 1985)”.
It is very difficult to identify the difference between type II and type III bone, from a histological and perceptive point of view (Trisi & Rao 1999).
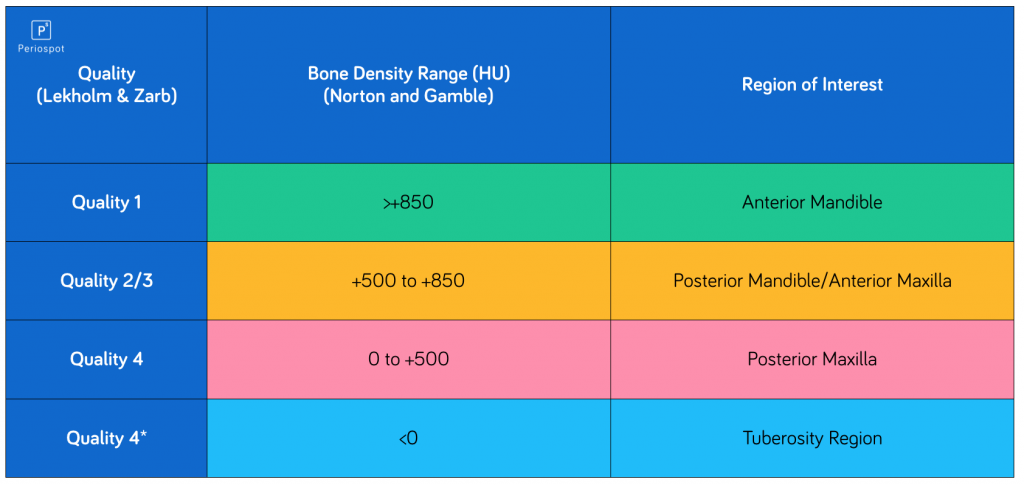
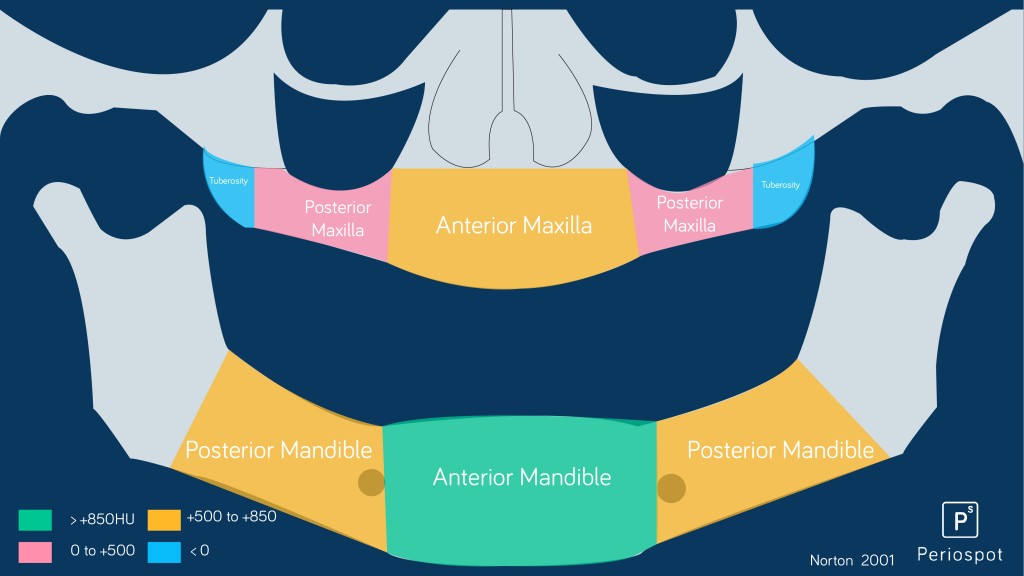
There is a direct correlation between Hounsfield units and bone quality (Norton 2001, Coutant 2014). Depending on the region of interest, there will be different bone quality and different expected Hounsfield units.
Also depending on the region where the immediate loading is performed, there will be different success rates (De Bruyn 2014).
Immediate loading in the anterior mandible, is described as the modality with highest success rate.
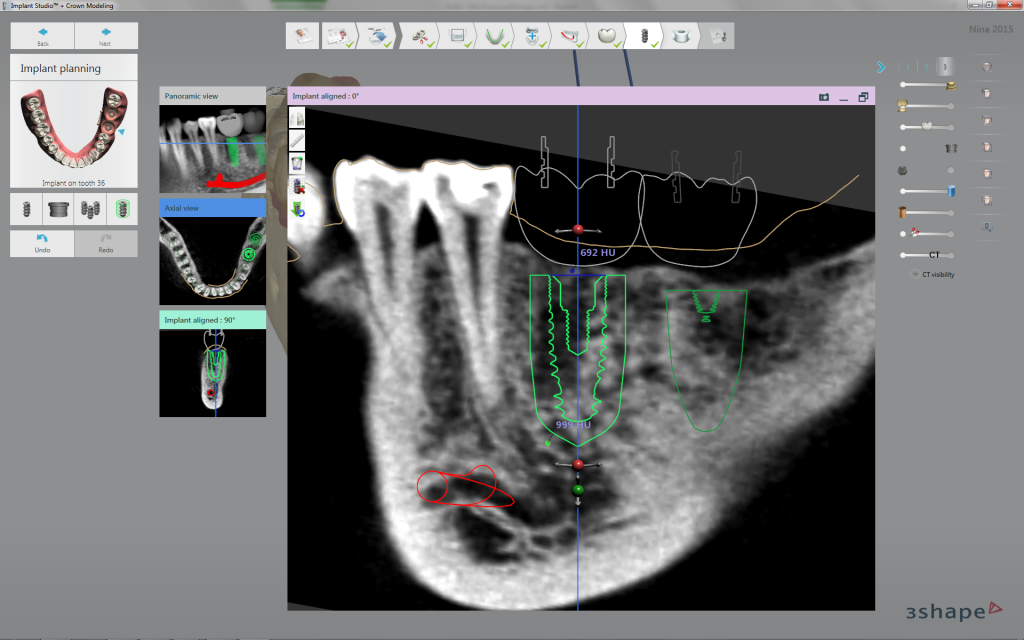
The use of the CT is mandatory to obtain the Hounsfield units (Coutant 2014). Nowadays we have a vast variety of softwares that can aid us to get the Hounsfield units.
We should consider very seriously the new software that allows merging an intraoral scanning and CT scans. 3Shape Implant Studio and CoDiagnostix® are an example of a software that integrates the possibility of merging a digital impression and a CT scan.
3Shape Implant Studio also provides the Hounsfield units of the bone where we decide to place the fixture.
Nailing an immediate loading case. The RFA device (Osstell®).
It has already been said that implant stability is mandatory to perform an immediate loading.
Primary stability can be evaluated by:
– Percussion tests
– Radiographic interpretation
– Insertion torque
– Sensations of the operator
– RFA (Resonance Frequency Analysis) or Osstell®
In this video you can see how Osstell® IDX works:
Resonance frequency analysis, was described 20 years ago by Meredith (Meredith 1996).
They evaluated the stiffness of the bone-implant complex, by using a self-curing resin.
I did a similar experiment at home, and this was the result:
But what ISQ values should we consider optimal, when we want to perform immediate loading?
These are the recommended values:
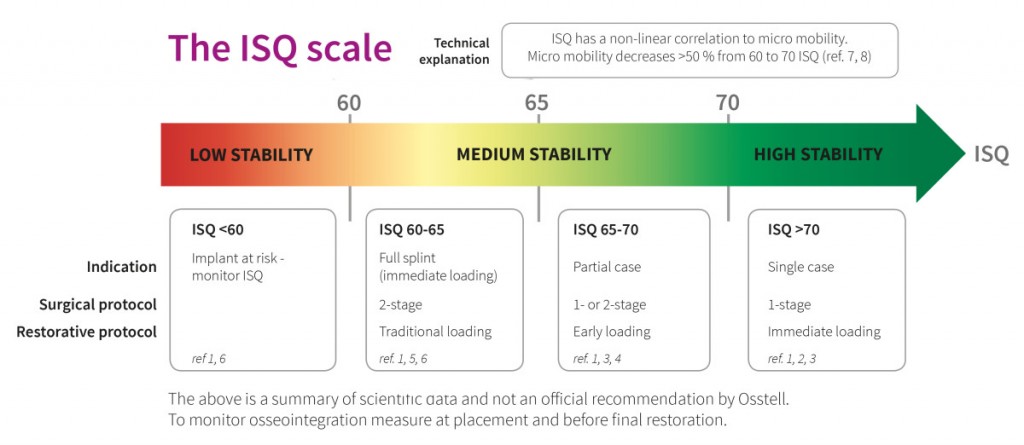
“Some emphasis should be done on implants with an ISQ >60. They can be immediattly loaded, but they should be splinted (Östman 2008)”.
If we are considering immediate restoration of single implants, a minimum of 70 ISQ is recommended (Kokovic 2012).
Osstell has an enormous scientific database. You can check the whole updated database here.
We can also monitorize the implants during the healing phase. When the ISQ drops (eg to a 50 ISQ value), we can leave that implant undisturbed and free from loading, till it gets an acceptable ISQ value after 1 or 2 months (Glauser 2004).
Conclusions
I tried to gather important information about immediate loading and I have to say that it is impossible to make it in just a blog post.
In a near future I will go deep into some other factors, like restorative aspects, patient-related risks (smokers mainly) and other points that may influence the outcome of an immediate loading protocol.
But here are some keypoints about immediate loading (chung 2011) :
– Bone quality and quantity should be appropriate.
– The rate of bone formation in a given region of the jaw should be considered.
– If required, extractions should be atraumatic.
– Initial implant stability (torque at the time of placement) at the time of surgery is crucial. In these
– Implant positioning should be prosthodontically driven.
– All forms of parafunctional habits should be avoided.
– Caution should be taken in patients with specific and recent (within two years) systemic conditions.
– Implants should not be placed into extraction sockets if they are currently infected.
– Balanced occlusion against natural teeth or prosthesis should be ensured.
– A minimum of 32 N·cm of torque should be used at the time of implant placement (although some protocols suggest torques as low as 25 N·cm).
– The implant system should be conducive to high primary stability/initial torque.
– Splinting of implants (and cross-arch stabilization) should be performed when possible.
– Prosthodontic rehabilitation should be balanced and passively fitting, and, if possible, a nonfunctional occlusal scheme should be implemented.
– Rough surfaced rather than smooth surfaced implants should be used.
– Hounsfield units should be measured when the case is being planned. Below 500 HU we should only consider for splinted implants.
– Osstell® is proven to be a noninvasive device to predict the outcome of the immediate loading. Remember that an ISQ<60 is a red light.
– Between week 1 and week three after implant placement, we should avoid manipulating the implants.
But there are many other factors that we have to consider before an immediate loading.
What are yours?
Do you prefer other approach rather than immediate loading?
Do you still consider immediate loading a nonreliable and predictable option?
What do you think is the future of immediate loading?
Recommended Book
Bibliography
Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003 Sep;18(5):641–51.
Berglundh T, Abrahamsson I, Lang NP, Lindhe J. De novo alveolar bone formation adjacent to endosseous implants. Clinical Oral Implants Research. 2003 Jun;14(3):251–62.
Brizuela-Velasco A, Álvarez-Arenal Á, Gil-Mur FJ, Herrero-Climent M, Chávarri-Prado D, Chento-Valiente Y, et al. Relationship Between Insertion Torque and Resonance Frequency Measurements, Performed by Resonance Frequency Analysis, in Micromobility of Dental Implants. Implant Dentistry. 2015 Oct;24(5):607–11.
Buser D, Weber HP, Bragger U. The treatment of partially edentulous patients with ITI hollow-screw implants: pre- surgical evaluation and surgical procedures. Int J Oral Maxillofac Implants 1990: 5: 165–175.
Chung S, McCullagh A, Irinakis T. Immediate Loading in the Maxillary Arch: Evidence-Based Guidelines to Improve Success Rates: A Review. Journal of Oral Implantology. 2011 Oct;37(5):610–21.
Coutant JC, Seguela V, Hauret L. Assessment of the correlation between implant stability and bone density by computed tomography and resonance frequency analysis in fresh cadavers. … Journal of Oral & …. 2014.
De Bruyn H, Raes S, Ostman P-O, Cosyn J. Immediate loading in partially and completely edentulous jaws: a review of the literature with clinical guidelines. Periodontol 2000. 2014 Oct;66(1):153–87.
Gallucci G, Benic G, Eckert S, Papaspyridakos P, Schimmel M, Schrott A, et al. Consensus Statements and Clinical Recommendations for Implant Loading Protocols. Int J Oral Maxillofac Implants. 2014 Jan;29(Supplement):287–90.
Glauser R, Sennerby L, Meredith N, Ree A, Lundgren A, Gottlow J, et al. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs. failing implants. Clinical Oral Implants Research. 2004 Aug;15(4):428–34.
Karoussis IK, Müller S, Salvi GE, Heitz-Mayfield LJA, Brägger U, Lang NP. Association between periodontal and peri‐implant conditions: a 10‐year prospective study. Clinical Oral Implants Research. Munksgaard International Publishers; 2004 Feb 1;15(1):1–7.
Kokovic V, Jung R, Feloutzis A, Todorovic VS, Jurisic M, Hämmerle CHF. Immediate vs. early loading of SLA implants in the posterior mandible: 5-year results of randomized controlled clinical trial. Clinical Oral Implants Research. 2012 Dec 21;25(2):e114–9.
Ledermann, P. (1979) [complete denture support in edentulous problem mandibles with help from 4 titanium plasma-coated pdl screw implants]. Schweizerische Monatsschrift fur Zahnheilkunde = Revue mensuelle suisse d’odonto-stomatologie/ SSO 89: 1137–1138.
Lekholm & Zarb. Patient selection and preparation. Quintessence; 1985;:199–209.
Lindhe J, Meyle J, on behalf of Group D of the European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. Journal of Clinical Periodontology. 2008 Sep;35:282–5.
Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant‐tissue interface using resonance frequency analysis. Clinical oral implants …. 1996.
Norton MR, Gamble C. Bone classification: an objective scale of bone density using the computerized tomography scan. Clinical Oral Implants Research. Munksgaard International Publishers; 2001 Feb;12(1):79–84.
ÖStman PO. Immediate/early loading of dental implants. Clinical documentation and presentation of a treatment concept. Periodontol 2000. 2008.
Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micromotion on bone-dental implant interface: Review of experimental literature. J Biomed Mater Res. 1998;43(2):192–203.
Touati B, Guez G. Immediate implantation with provisionalization: from literature to clinical implications. Pract Proced Aesthet Dent. 2002 Nov;14(9):699–707–quiz708.
Trisi P, Rao W. Bone classification: clinical-histomorphometric comparison. Clinical Oral Implants Research. 1999 Feb;10(1):1–7.
Turkyilmaz I, Hoders AB. Immediate Loading in Implant Dentistry. In: Current Concepts in Dental Implantology. InTech; 2015. pp. 1–22.
Wismeijer D, Buser D, Belser U. ITI Treatment Guide, Vol 4: Loading Protocols in Implant Dentistry. Berlin: Quintessence; 2010.